To keep healthcare human, we need better tech
The Fast Company Impact Council is an invitation-only membership community of leaders, experts, executives, and entrepreneurs who share their insights with our audience. Members pay annual dues for access to peer learning, thought leadership opportunities, events and more. While virtual doctor visits were available prior to 2020, the COVID-19 pandemic kicked them into overdrive: From 2018-2022, the percentage of American hospitals offering telehealth jumped over 14% to 86.9%. In 2021, McKinsey reported that the use of virtual care had stabilized at 38 times higher than before the pandemic. That same year, 85% of doctors offered it and 37% of adults surveyed had used it in the past year. In less than a decade, telehealth has gone from care alternative to industry staple. But with patients and providers increasingly dissatisfied with the quality of care, is this a positive development? It can be. As the CEO of Sollis Health, a 24/7 concierge medical membership, I’ve seen how telehealth can be leveraged alongside features like premium tech-based services, healthcare personalization, and powerful proactive care to prioritize patient experience, support providers, and boost health outcomes—because “high-tech” and “human-centered” don’t have to be mutually exclusive. Premium tech-based services More than ever, time is a luxury for both patients and healthcare providers: Patients are waiting longer for care while overworked providers are slowed down by administrative burdens and staffing shortages. This lack of time contributes to burnout on both sides, with a 2022 poll revealing that fewer than half of Americans feel that the healthcare system is “generally handled well.” On the provider side, a 2024 survey showed that 48.2% of physicians reported experiencing at least one symptom of burnout. Tech-based services could help fill these gaps, alleviating these pressures on both sides. AI is just one example. By automating administrative tasks, streamlining preventive care, and even playing a role in diagnostics—like reading MRIs or X-rays—a smart rollout of AI could free providers to spend more intentional time with patients while making care more efficient and effective by finding cancer sooner and making precision medicine more comprehensive. Healthcare personalization Women are more likely to die from heart attacks—and yet, because of medical biases, they are also more likely to be misdiagnosed. While a one-size-fits-all approach to healthcare has long been the norm, care that tailors medical treatments and interventions to the unique needs of individual patients not only improves health outcomes, but streamlines them, too. From simply making sure patients are comfortable before, during, and after exams, to providing access to wearables like Zio patches, targeted cancer diagnostics, and seamless care navigation, personalized healthcare can save time and money by enhancing prevention and refining diagnostics. It can also improve engagement and compliance: Healthcare strategies specifically tailored to an individual’s needs makes patients feel more understood and cared for overall. Powerful proactive care You’re probably already familiar with preventive care, which research shows could reduce premature cancer deaths by about 40%. Proactive care broadens preventive care’s reach by deepening the connection between patients and providers with more and better communication while encouraging traditional preventive measures like health education, lifestyle changes—like quitting smoking or balanced eating habits—and screenings for conditions like heart disease, diabetes, and cancer. Unfortunately, in the United States only slightly more than half of recommended healthcare interventions are provided during the course of normal care, often due to a lack of time. Technological advances in preventive care have so much to offer, especially in terms of access. Thanks to the time-savings of telehealth, AI-driven diagnostics, app-based medical education and care, wearables, and more, proactive care becomes more accessible to those who need it, including at-risk patients, patients managing chronic conditions, and others who would benefit from the convenience of higher-tech care. The future of healthcare is human-centered Finding solutions to a healthcare system that’s become too complex, transactional, and onerous doesn’t mean ignoring technologies like telehealth—it means striking the delicate balance between the human touch and the cutting edge. Whether it’s as simple as a warmer bedside manner or as advanced as AI-driven predictive analytics, human-centered healthcare is not just possible, but necessary, in this evolving landscape. Brad Olson is CEO of Sollis Health.

The Fast Company Impact Council is an invitation-only membership community of leaders, experts, executives, and entrepreneurs who share their insights with our audience. Members pay annual dues for access to peer learning, thought leadership opportunities, events and more.
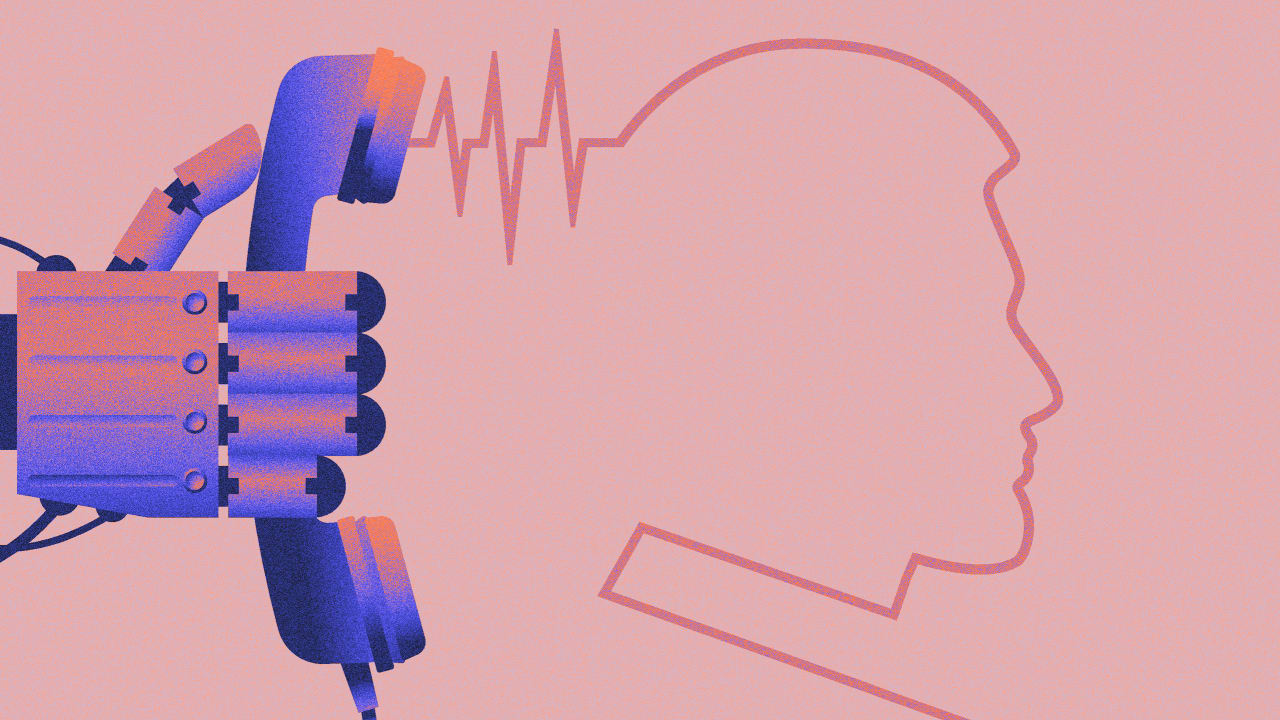
While virtual doctor visits were available prior to 2020, the COVID-19 pandemic kicked them into overdrive: From 2018-2022, the percentage of American hospitals offering telehealth jumped over 14% to 86.9%. In 2021, McKinsey reported that the use of virtual care had stabilized at 38 times higher than before the pandemic. That same year, 85% of doctors offered it and 37% of adults surveyed had used it in the past year. In less than a decade, telehealth has gone from care alternative to industry staple. But with patients and providers increasingly dissatisfied with the quality of care, is this a positive development?
It can be. As the CEO of Sollis Health, a 24/7 concierge medical membership, I’ve seen how telehealth can be leveraged alongside features like premium tech-based services, healthcare personalization, and powerful proactive care to prioritize patient experience, support providers, and boost health outcomes—because “high-tech” and “human-centered” don’t have to be mutually exclusive.
Premium tech-based services
More than ever, time is a luxury for both patients and healthcare providers: Patients are waiting longer for care while overworked providers are slowed down by administrative burdens and staffing shortages. This lack of time contributes to burnout on both sides, with a 2022 poll revealing that fewer than half of Americans feel that the healthcare system is “generally handled well.” On the provider side, a 2024 survey showed that 48.2% of physicians reported experiencing at least one symptom of burnout.
Tech-based services could help fill these gaps, alleviating these pressures on both sides. AI is just one example. By automating administrative tasks, streamlining preventive care, and even playing a role in diagnostics—like reading MRIs or X-rays—a smart rollout of AI could free providers to spend more intentional time with patients while making care more efficient and effective by finding cancer sooner and making precision medicine more comprehensive.
Healthcare personalization
Women are more likely to die from heart attacks—and yet, because of medical biases, they are also more likely to be misdiagnosed.
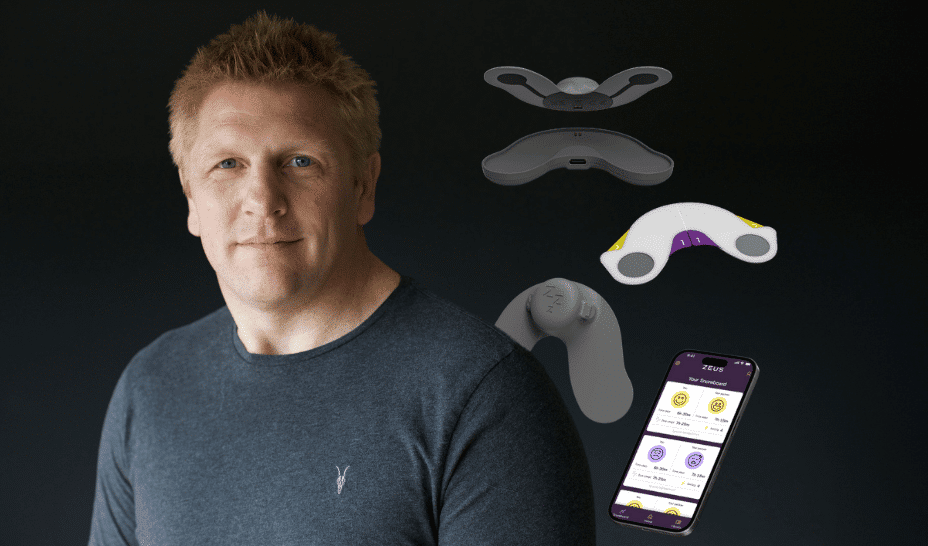
While a one-size-fits-all approach to healthcare has long been the norm, care that tailors medical treatments and interventions to the unique needs of individual patients not only improves health outcomes, but streamlines them, too. From simply making sure patients are comfortable before, during, and after exams, to providing access to wearables like Zio patches, targeted cancer diagnostics, and seamless care navigation, personalized healthcare can save time and money by enhancing prevention and refining diagnostics. It can also improve engagement and compliance: Healthcare strategies specifically tailored to an individual’s needs makes patients feel more understood and cared for overall.
Powerful proactive care
You’re probably already familiar with preventive care, which research shows could reduce premature cancer deaths by about 40%. Proactive care broadens preventive care’s reach by deepening the connection between patients and providers with more and better communication while encouraging traditional preventive measures like health education, lifestyle changes—like quitting smoking or balanced eating habits—and screenings for conditions like heart disease, diabetes, and cancer.
Unfortunately, in the United States only slightly more than half of recommended healthcare interventions are provided during the course of normal care, often due to a lack of time. Technological advances in preventive care have so much to offer, especially in terms of access. Thanks to the time-savings of telehealth, AI-driven diagnostics, app-based medical education and care, wearables, and more, proactive care becomes more accessible to those who need it, including at-risk patients, patients managing chronic conditions, and others who would benefit from the convenience of higher-tech care.
The future of healthcare is human-centered
Finding solutions to a healthcare system that’s become too complex, transactional, and onerous doesn’t mean ignoring technologies like telehealth—it means striking the delicate balance between the human touch and the cutting edge. Whether it’s as simple as a warmer bedside manner or as advanced as AI-driven predictive analytics, human-centered healthcare is not just possible, but necessary, in this evolving landscape.
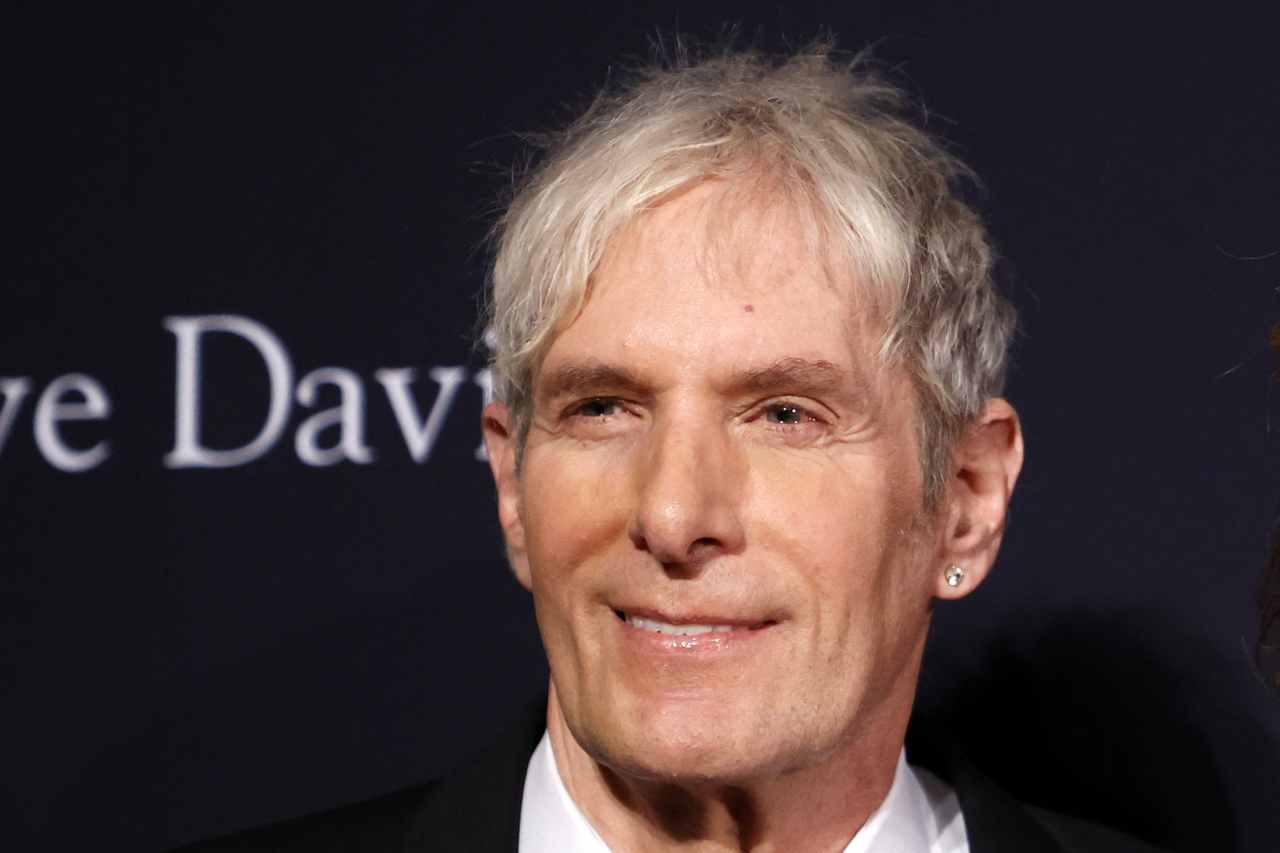
Brad Olson is CEO of Sollis Health.